Patients Struggle as Gaps in Kenya’s Social Health Authority Rollout Impact Access to Essential Care
By John Waithaka
Nairobi, Kenya – A recent survey has revealed alarming gaps in the rollout of Kenya’s Social Health Authority (SHA) and Social Health Insurance Fund (SHIF), leaving patients with non-communicable diseases (NCDs) struggling to access essential healthcare. Conducted by the Caucus of Patient-Led Organizations of Non-Communicable Diseases, the survey examined healthcare facilities across Nairobi, Kiambu, Meru, and Bomet Counties between October 24 and 25, 2024. Its findings expose significant barriers to healthcare access, including increased out-of-pocket costs, coverage limitations, and systemic delays that burden both patients and providers.
One major concern identified is the shift to out-of-pocket expenses for outpatient visits and drug refills, which were previously covered under the National Health Insurance Fund (NHIF). For many patients with chronic conditions like cancer, diabetes, and cardiovascular disease, this change has imposed a financial strain that limits access to primary care services. The survey findings underscore that without swift reforms, these issues threaten to worsen healthcare access disparities for vulnerable populations.
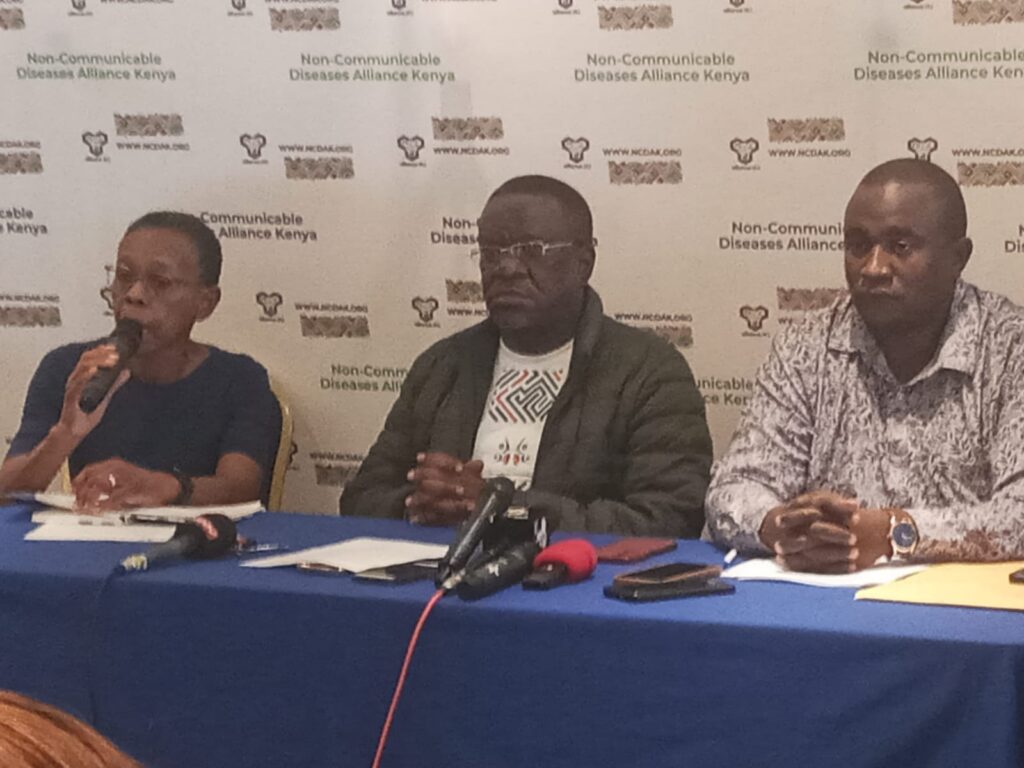
Patients in public hospitals, such as Kenyatta National Hospital and Kenyatta University Referral Hospital, reported hours-long waits due to frequent system delays and technical failures, with “system hangs” exacerbating patient frustration and distress. These inefficiencies impact critical services like diagnostic imaging and specialized procedures, creating backlogs that prevent timely care. “For patients facing conditions like heart disease, cancer, or other chronic illnesses, every delay can mean the difference between manageable symptoms and a crisis,” said Evans M. Majau, Chair of the Caucus of Patient-Led Organizations of NCDs. “Patients with non-communicable diseases simply can’t afford to keep waiting.”
Private facilities have restricted SHA coverage to specific groups—typically civil servants—leaving many patients forced to cover costs out of their own pockets. Patients with severe illnesses who don’t fit into narrow eligibility groups have been particularly hard-hit by SHA’s rollout limitations. In rural areas, SHA’s limitations are even starker. Mission hospitals like Tenwek, which provide essential services to underserved populations, reported that they have no SHA coverage at all. Without this support, many rural patients face insurmountable costs if they need complex procedures, such as cardiac surgeries, that only select facilities in Kenya can perform.
The survey highlighted additional issues that have compounded these problems. Out-of-pocket expenses for outpatient services and medication refills, previously covered under NHIF, now pose an added burden for NCD patients. The accumulation of unpaid NHIF bills, combined with unclear SHA benefit structures, has led to hesitancy among healthcare providers to offer SHA services, as they fear reimbursement delays or potential exclusions. SHA has also suspended coverage for overseas treatments, leaving many patients without options for specialized care that is unavailable within Kenya. A lack of information about SHA benefits, premium structures, and eligibility requirements has left many patients unprepared to navigate the new system, creating confusion and stress for those seeking care.
The Caucus of Patient-Led Organizations of NCDs has issued an urgent call for action to address these issues, urging the Ministry of Health and SHA Management to resume overseas treatment coverage for patients requiring specialized care that is unavailable locally, clarify and publicize SHA benefit structures to ensure transparency and rebuild patient trust in the healthcare system, address system failures promptly to improve the efficiency of registration, preauthorization, and payment processes, settle outstanding NHIF debts to allow service providers to confidently accept SHA patients without fearing financial losses, launch public awareness campaigns to increase patient understanding of SHA benefits and financing options, and engage patient organizations and civil society to ensure that SHA implementation includes patient-centered solutions.
“The survey findings reveal critical gaps in SHA’s ability to serve Kenyan patients effectively, especially those facing chronic and complex conditions like cancer, diabetes, and cardiovascular diseases,” said Majau. “The SHA rollout must prioritize transparency, access to specialized care, and patient inclusion to fulfill the promise of universal health coverage in Kenya. We urge the Ministry of Health and SHA leaders to engage with patient voices and take swift, corrective action to address these issues.”
The Caucus reaffirms its commitment to advocating for the health needs of all Kenyans and believes that, through collaboration and informed action, an equitable healthcare system that ensures timely, quality care for every patient is achievable. The challenges ahead are significant, but so is the determination of patient advocates to see meaningful improvements for those in need of care.





